Dr Grace Lui Chung-yan (1st, right) from the Department of Medicine and Therapeutics; Professor Benny Zee Chung-ying (2nd, left) from the Centre for Clinical Research and Biostatistics, and other research team members from CU Medicine
Estimating the risk of heart disease in people living with HIV
Although there are existing calculators for predicting the risk of coronary artery disease in an individual, they are often inaccurate, as they fail to take into account many host characteristics, including ethnicity and underlying medical conditions such as HIV.
The Centre for Clinical Research and Biostatistics, the Department of Medicine and Therapeutics, and the Department of Imaging and Interventional Radiology from the CU Medicine have evaluated the effectiveness of a simple tool – Automatic Retinal Image Analysis (ARIA) technology – for assessing cardiovascular risk in people living with HIV. Results showed the model, which incorporates both retinal characteristics and traditional cardiovascular risk factors, has both a sensitivity and a specificity of over 90% in assessing the presence of coronary atherosclerosis and obstructive coronary artery disease. The findings have been published in the medical journal PLOS ONE.
A predictive model is needed to precisely assess the risk of cardiovascular disease in people living with HIV
People living with HIV have twice the risk of healthy individuals of developing cardiovascular disease. They also have a higher prevalence of hypertension and diabetes, contributing risk factors to cardiovascular diseases. Interventions are available to reduce the risk of coronary artery disease in at-risk individuals, but a simple, accurate tool is needed to identify the individual risks among them.
Dr Grace Lui Chung-yan, Clinical Associate Professor (honorary) from the Department of Medicine and Therapeutics at CU Medicine, said, “Current clinical guidelines recommend that people living with HIV have regular cardiovascular risk screenings. Though there are various traditional risk prediction models, none has been developed for HIV-infected populations, so there is a need to look for the best model for them.”
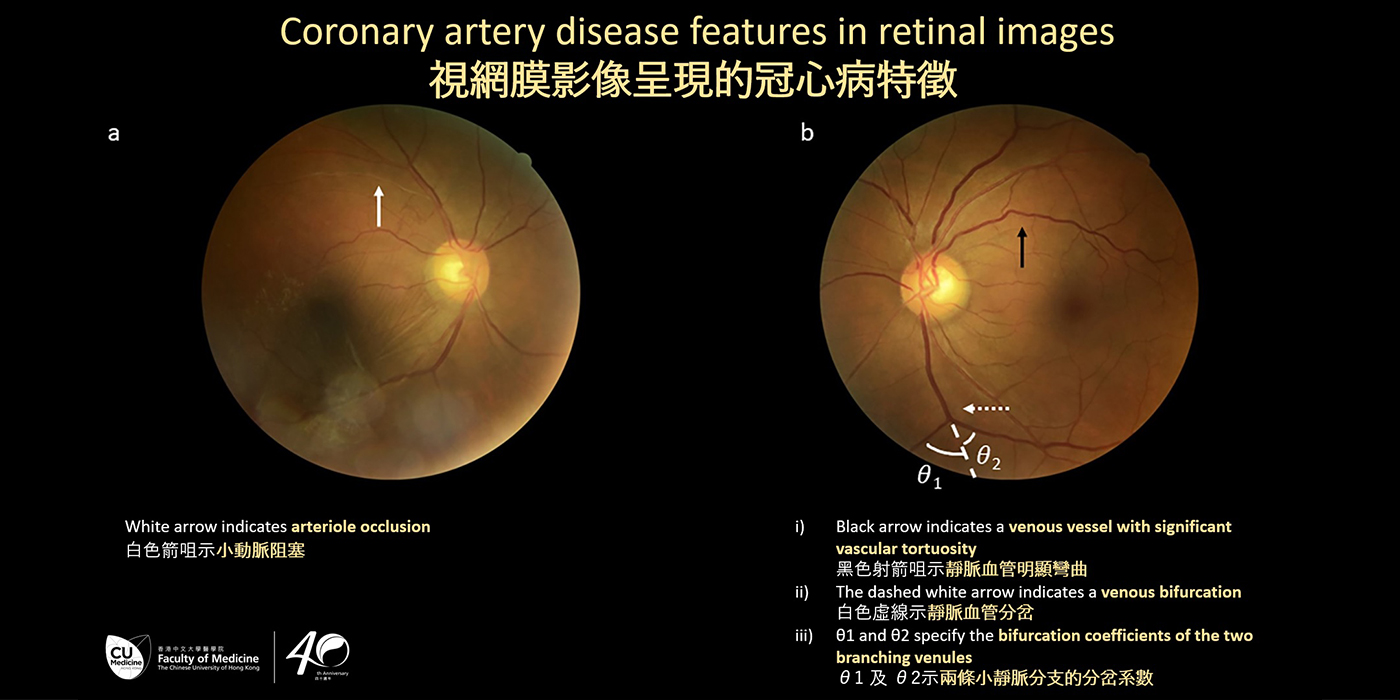
Professor Benny Zee Chung-ying, Director of the Centre for Clinical Research and Biostatistics at The Jockey Club School of Public Health and Primary Care at CU Medicine, added, “Recent studies have shown retinal image characteristics are closely linked with multiple cardiovascular risk factors and major cardiovascular events. Features including arteriolar and venular calibre, curvature tortuosity and branching complexity have been shown to have associations with coronary artery disease.”
CU Medicine’s combined prediction model achieved over 90% of sensitivity and specificity in estimating risk of heart disease in HIV patients
The CU Medicine research team recruited 115 people living with HIV who have one or more risk factors for cardiovascular disease to evaluate the performance of a model combining traditional cardiovascular risk factors and retinal characteristics. Among them, 71 (62%) had coronary atherosclerosis and 23 (20%) had obstructive coronary artery disease, as detected by computed tomography (CT) scan. All participants had retinal images captured by a non-mydriatic retinal camera. These images were then analysed using machine learning and deep learning techniques.
The results showed the model incorporating both retinal characteristics and traditional cardiovascular risk factors had both a sensitivity and a specificity of over 90% in assessing the presence of the two types of heart disease (see details in Tables 1 and 2 in the appendix).
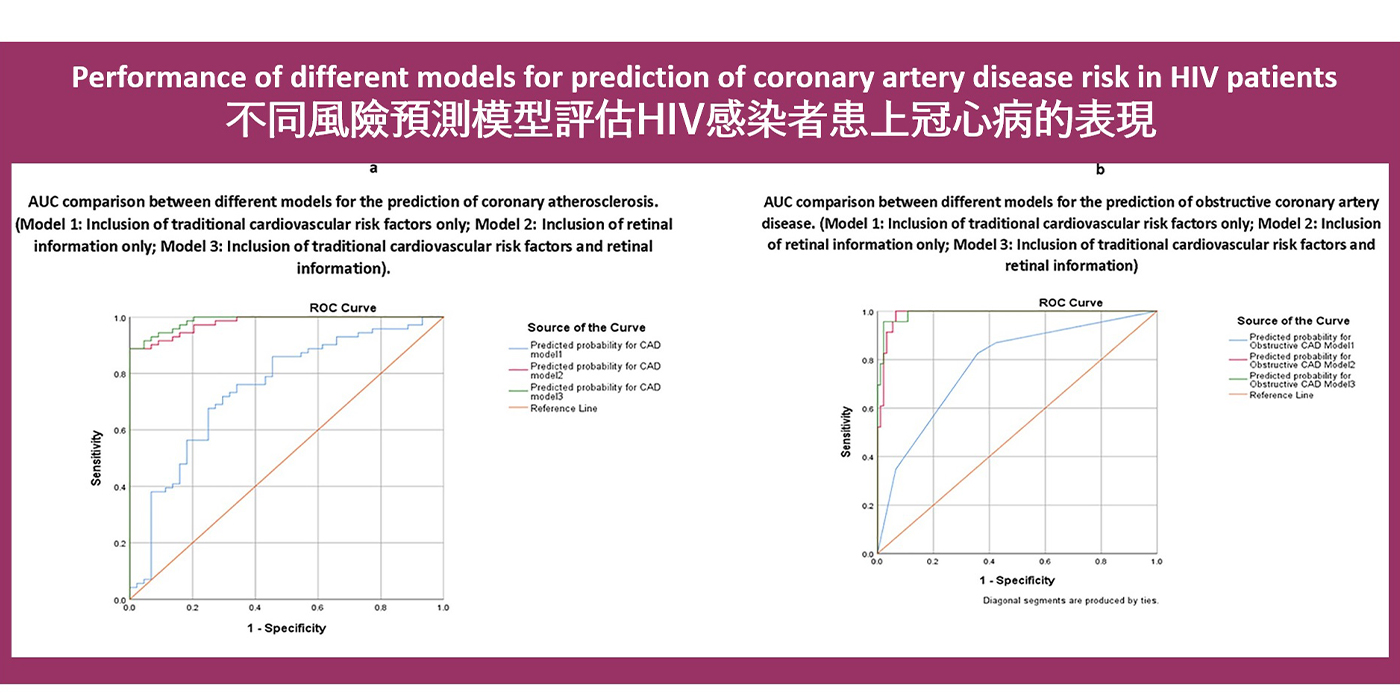
Professor Zee remarked: “This study has demonstrated the role that automatic retinal image analysis, a simple, efficient tool, can have in assessing the risk of heart disease in at-risk individuals. Statistical models incorporating retinal characteristics performed the best, and were significantly better than traditional risk prediction tools at predicting coronary artery disease, and in particular obstructive coronary artery disease.”