Awe-inspiring tissue regeneration
Professor Barbara Chan rekindles patients’ hope for cartilage repair
On 27 November, Professor Barbara Chan delivered her inaugural lecture as the Au Chik Ko and Au Leung Shook Yin Professor in Biomedical Engineering at the CUHK Medical Centre. The Kai Chong Tong Auditorium was packed with audience members, who came to share her joy in the endowed professorship and learn from her lecture “Building Tissues from Scratch—Technologies, Sciences, Applications and Challenges”.
The professorship is named after the parents of Ms Betty Au (1971/UC/Social Work), Au Chik Ko and Au Leung Shook Yin, and aims to push back the frontiers of biomedical engineering and regenerative medicine.

Professor Chan is one of the world’s pioneers in cartilage tissue engineering. “Our vision is to benefit patients who suffer from tissue dysfunctions by developing safe, effective, personalised tissue engineering and regenerative medicine solutions,” she said.
She is currently a professor in CUHK’s School of Biomedical Science; Institute of Tissue Engineering; and Department of Biomedical Engineering. She obtained her bachelor’s degree in Biochemistry and her PhD in Surgical Science from CUHK, and a Postdoctoral Fellowship in Laser Medicine at the Massachusetts General Hospital in the US. She worked on the Biomedical Engineering programme of The University of Hong Kong (HKU) before joining CUHK.
An engineering solution to medical conditions
About 528 million people worldwide were living with osteoarthritis in 2019, according to the World Health Organisation, which is an increase of 113% since 1990. The knee joint is the most common site for degenerative joint diseases such as osteoarthritis, a condition that causes pain, swelling and stiffness. Without blood vessels, cartilage cannot heal on its own once injured. In the worst scenario, the patient’s knee joint needs replacing by an artificial joint.
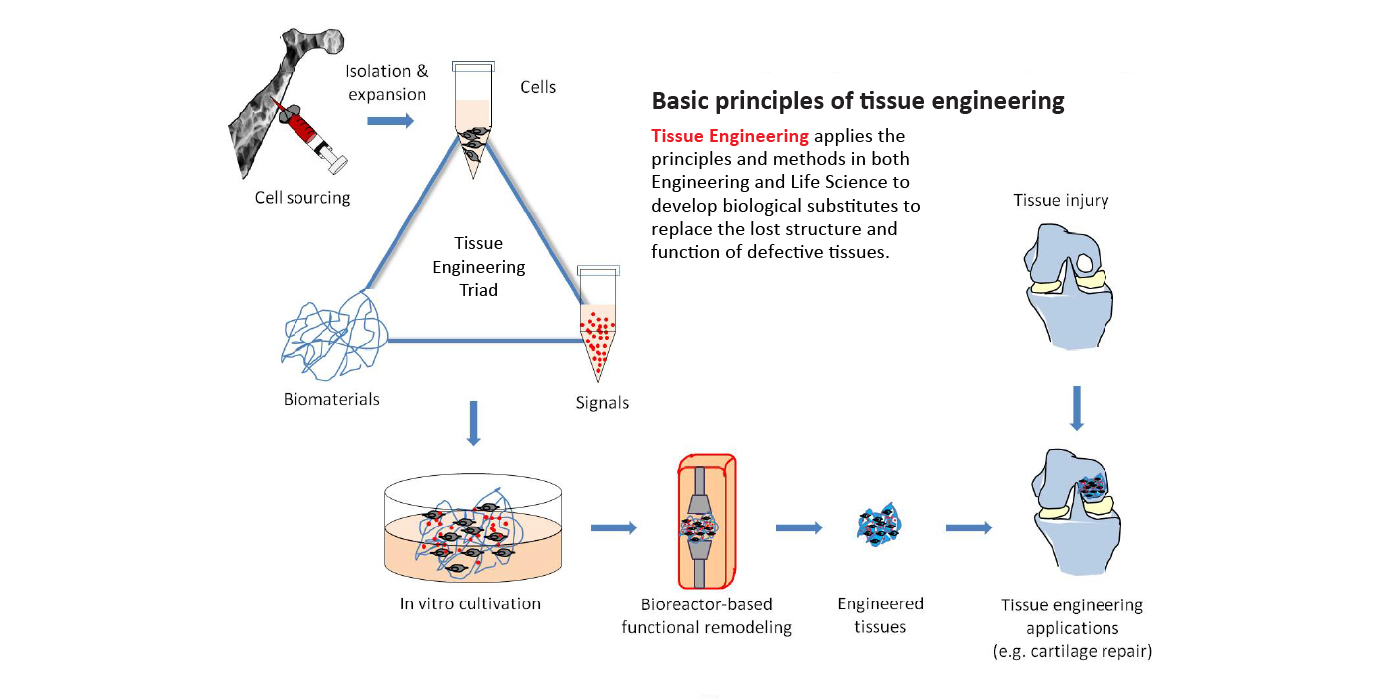
Professor Chan’s team has developed platform technologies to enable the research and development of biological substitutes to replace tissue. Their ultimate goal is to bioengineer clinically usable living tissues to replace defective ones. By integrating different technologies, they have developed bioengineered complex tissues such as the engineered osteochondral tissue (eOCT) for cartilage regeneration. During her lecture, Professor Chan shared the development roadmap of eOCT, from proof of concept to pre-clinical evaluation, from cadaveric studies on surgical implantation to process validation for Good Manufacturing Practice (GMP), now preparing for first-in-human clinical trials.
Surgical procedures such as microfracture and autografting can be used to treat cartilage damage but there are significant drawbacks. Microfracture involves drilling tiny holes into the bones underlying the damaged cartilage, but cartilage repaired this manner is of poor quality and will degenerate quickly. Autografting involves harvesting a graft from a part of the joint to replace the damaged cartilage and is required as the clinical golden standard. However, owing to the severe side effects, such as chronic pain and degeneration due to the injured autograft donor site, this procedure is no longer offered by surgeons.
“The use of these regenerative complex tissue plugs allows orthopedic surgeons to use the minimal invasive arthroscopy procedure to repair cartilage damage without the need to hurt the patients’ own cartilage, like the existing surgical procedures do. We grow the cartilage tissues in vitro using the patients’ own stem cells and use the engineered cartilage to replace the damaged tissues. We are now translating this technology for use on humans,” said Professor Chan. The performance of eOCT has been proven comparable with autograft transplantation in animal studies.

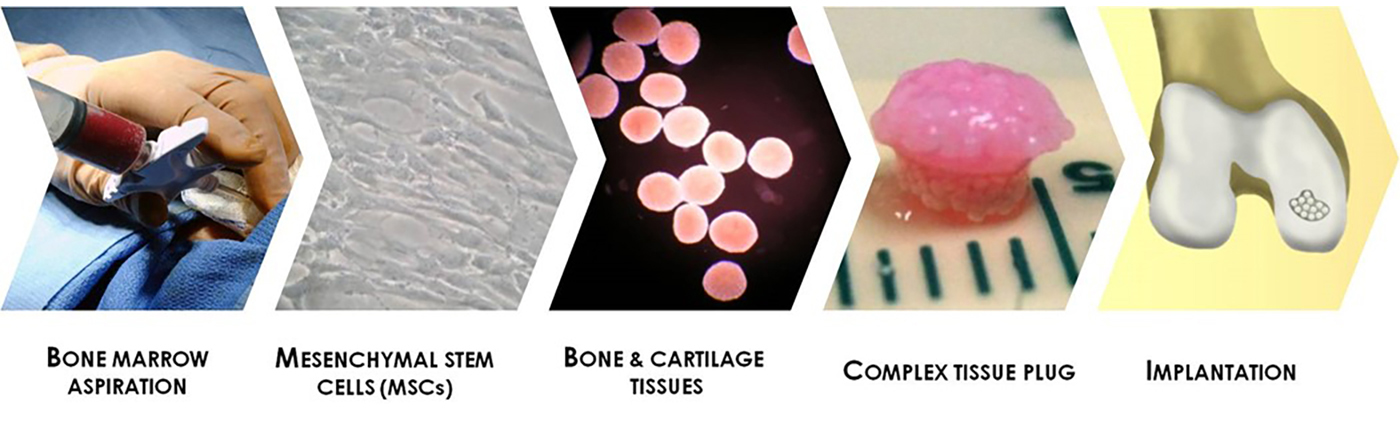
In order to translate the eOCT technology into clinical applications, Professor Chan’s team has established collaborations with multiple organisations and institutions for GMP manufacturing and associated services, and multiple hospitals for the subsequent clinical trial.
Building from strength to strength
With over 25 years of multidisciplinary research experience in tissue engineering and regenerative medicine, Professor Chan has established the Tissue Engineering Laboratory to improve the quality of life in patients through bioengineering biomaterials and stem cell-based tissues for personalised therapies. Her research interests include complex tissue engineering, natural biomaterials, organoids and tumoroids, mechano-regulation, cell-material interface, multiphoton microfabrication and micropatterning, as well as laser medicine.
Professor Chan is the first tissue engineering scientist to develop the associated technology to such an advanced stage. She was determined to develop better therapeutics for patients suffering from joint problems. Her team has overcome numerous technical limitations and pushed scientific frontiers to bridge this unmet medical need. Together with her business partner and previous PhD students and postdocs, Professor Chan has also co-founded a company to develop personalised tissue engineering-based Advanced Therapeutic Products (ATPs), an emerging industry in Hong Kong.
Her dream is to realise personalised cartilage regeneration within the healthcare system. “Someday in the future, patients with cartilage injuries may send their pre-stored stem cells from cell banks to professional tissue growth service providers for their made-to-order personalised eOCT as their tissue engineering option for arthroscopy implantation. Hopefully, the eOCT ATP will allow them to regain motility and enjoy their preferred lifestyles soon afterwards.”
Profile of Professor Barbara Chan
|
By Jenny Lau