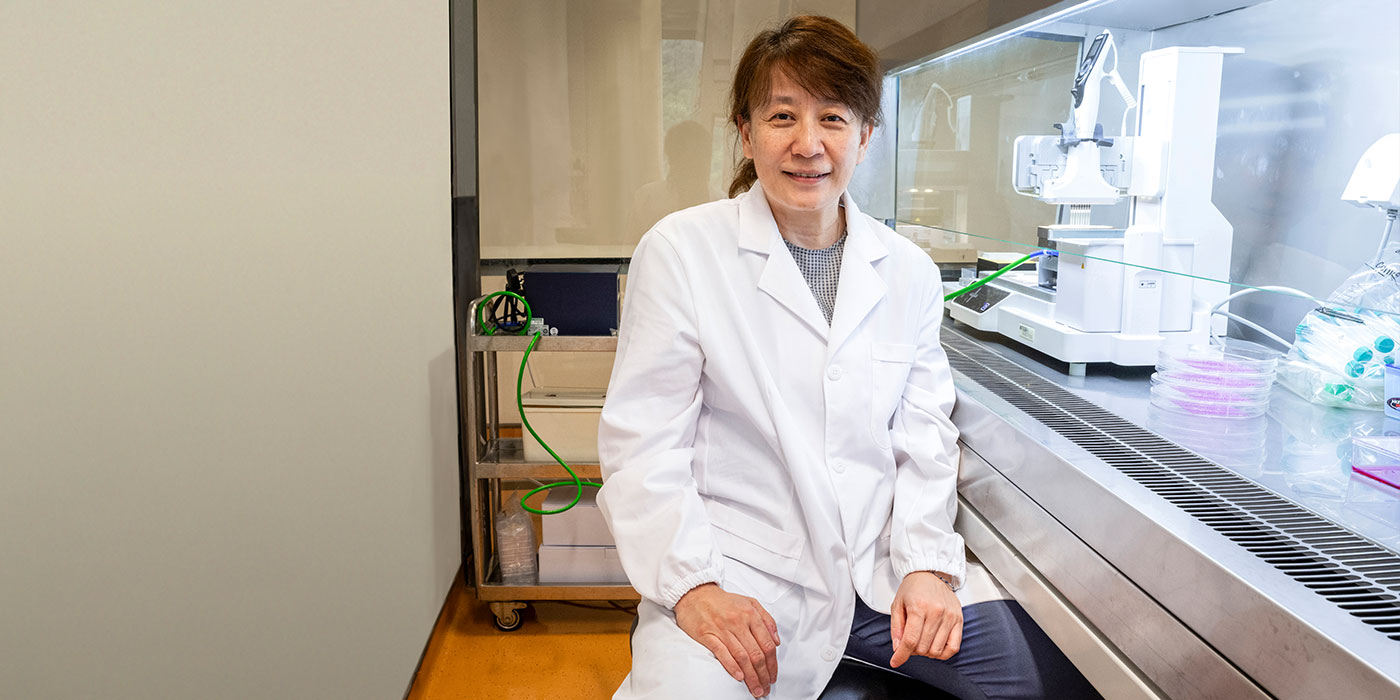
On passion and perseverance
Barbara Chan endeavours to use tissue engineering to heal patients
This is part two of our series on the seven CUHK teams that have won funding awards from the government’s Research, Academic and Industry Sectors One-plus (RAISe+) Scheme.
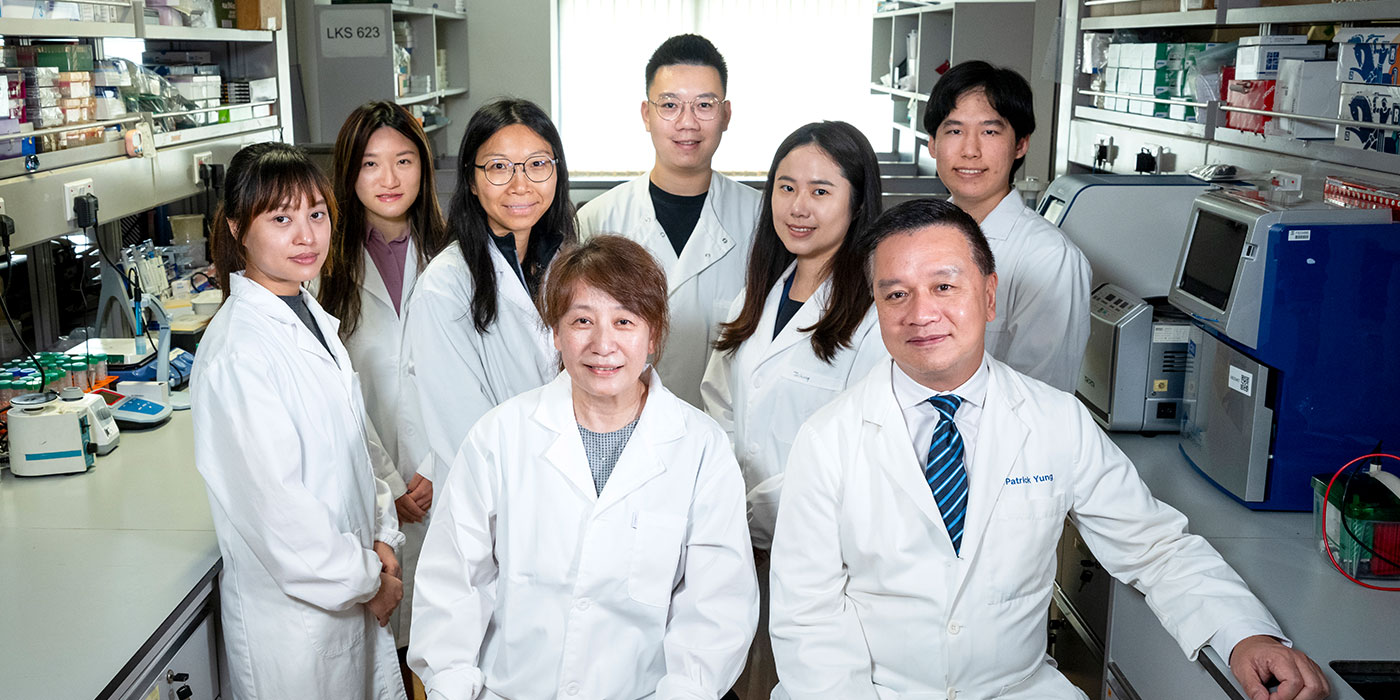
As one of the global pioneers in cartilage tissue engineering, Professor Barbara Chan of CUHK’s has been diving deep into tissue engineering and regenerative medicine research for over 25 years. She wants to benefit patients who suffer from tissue dysfunctions by developing safe, effective, personalised tissue engineering and regenerative medicine solutions.
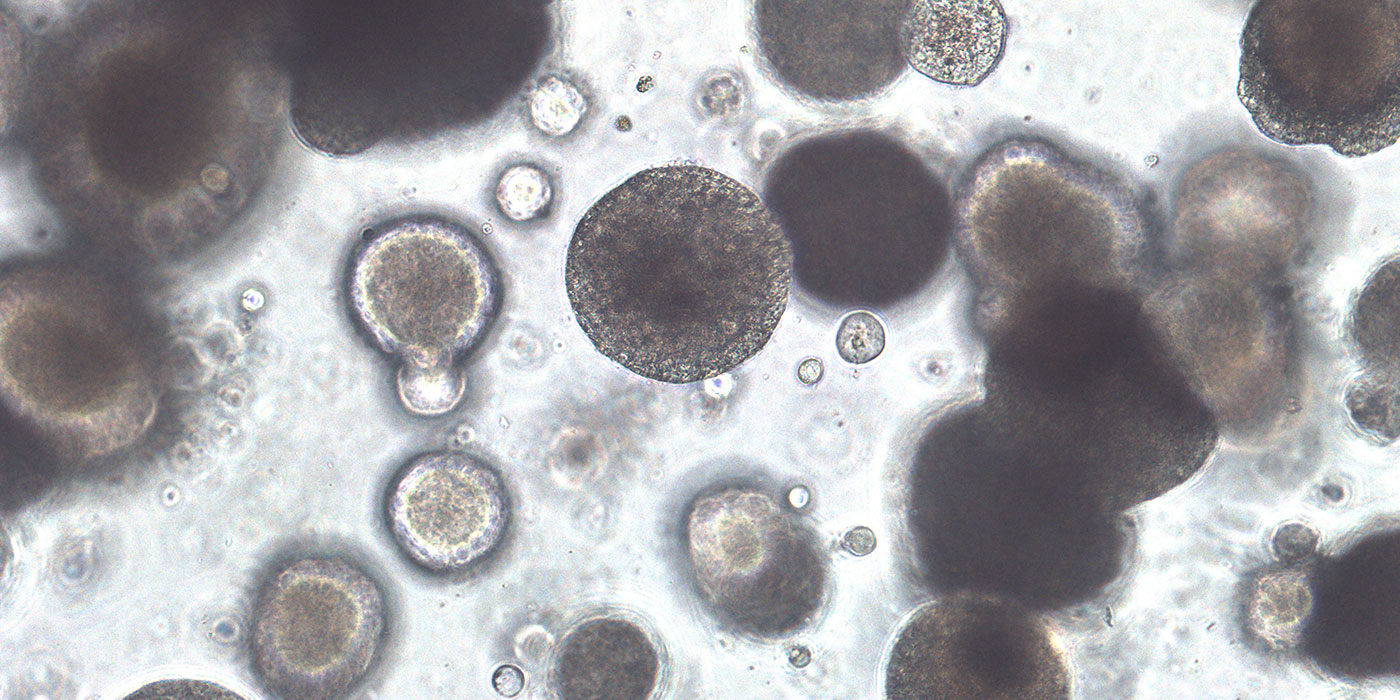
Professor Chan’s team strives to bioengineer clinically usable living tissues to replace defective ones. By integrating different technologies, they have developed bioengineered complex tissues such as engineered osteochondral tissue (eOCT) for cartilage regeneration. Her project “development of personalised advanced therapeutic products (ATPs)—eOCT for cartilage regeneration therapy” has been funded by the RAISe+ Scheme.
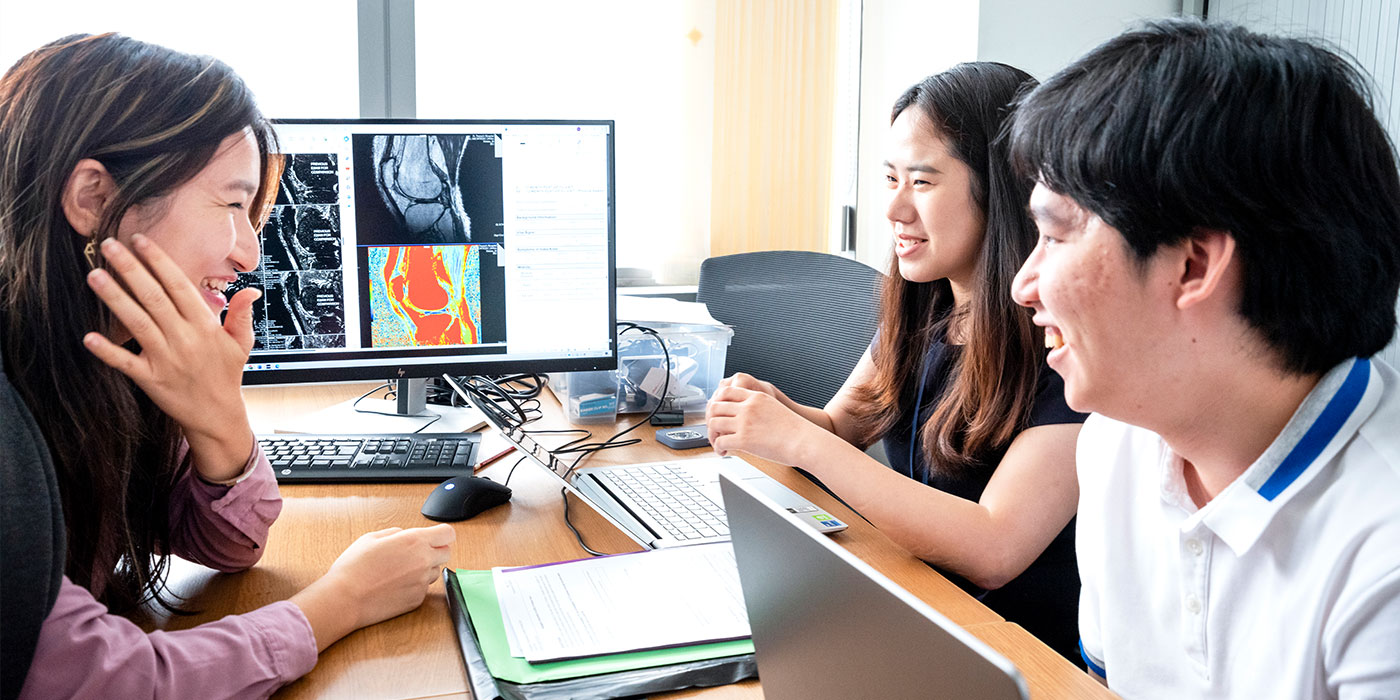
In close collaboration with the orthopaedic team led by Professor Patrick Yung of CU Medicine, Professor Chan is realising her roadmap of eOCT development: from proof of concept to pre-clinical evaluation, from cadaveric studies on surgical implantation to process validation for Good Manufacturing Practice (GMP), and now conducting first-in-human clinical trials in Prince of Wales Hospital and Queen Elizabeth Hospital.
“This is the best era for doing interdisciplinary translational research. Compared with other countries and regions, local scientists have more substantial funding and infrastructural support from the Hong Kong government,” she says.
Rekindling patients’ hope for cartilage repair
According to The Lancet, about 595 million people worldwide were living with osteoarthritis in 2020, up 132.2% since 1990. The knee joint is the most common site for degenerative joint diseases such as osteoarthritis, a condition that causes pain, swelling and stiffness. Without blood vessels, cartilage cannot heal on its own once injured. In the worst-case scenario, the patient’s knee joint needs to be replaced by an artificial one.
Professor Yung, who is responsible for the handling joint replacement cases in the Hospital Authority’s New Territories East cluster, says his team handles 1,000 cases per year but there are 4,000 to 5,000 cases on waiting list. “And the list is getting longer as our society is ageing rapidly,” he says. “Knee joint replacement is the most common orthopaedic surgery in Hong Kong. It takes around four to six years for patients to receive knee joint replacement surgery.”
Surgical procedures, such as microfracture and autografting, can be used to treat traumatic cartilage damage but there are significant drawbacks. Microfracture involves drilling tiny holes into the bones underlying the damaged cartilage, but cartilage repaired in this manner is of poor quality and will degenerate quickly. Autografting involves harvesting a graft from a part of the joint to replace the damaged cartilage and is the clinical gold standard. However, owing to the severe side effects, such as chronic pain and degeneration due to the injured autograft donor site, this procedure is no longer offered by surgeons.
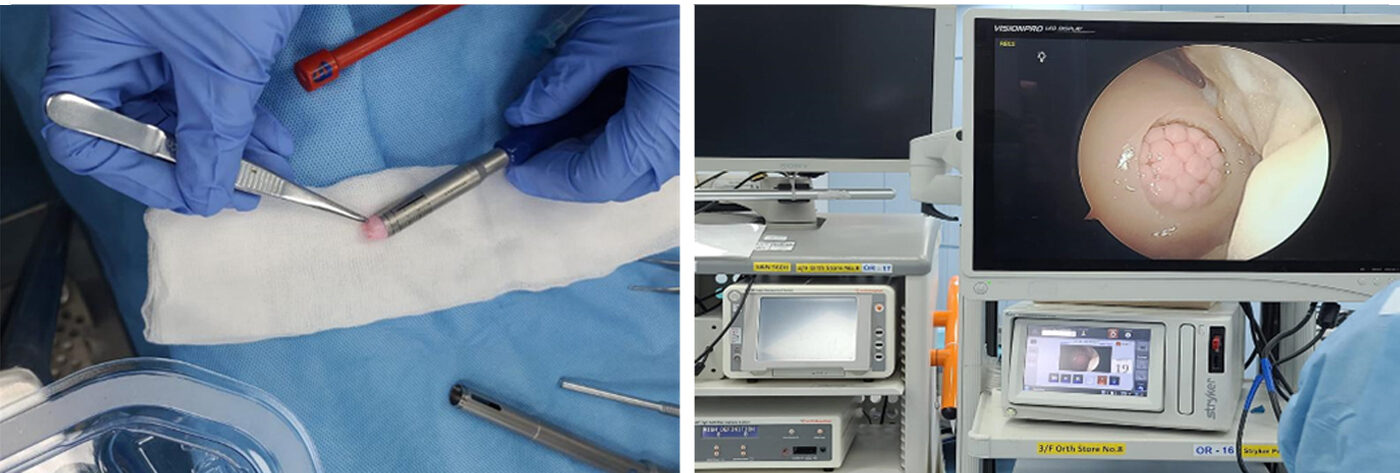
Professor Yung has been applying matrix-induced autologous chondrocyte implantation (MACI) for two decades, a procedure in which a patient’s own cells are used to regrow new cartilage for the knee joint. The patient’s harvested cells are placed onto a film trimmed by the surgeon for implantation into the damaged area to regrow new cartilage. “It usually takes more than 18 months to fill part of the defect area, but Professor Chan’s eOCT plug can completely fill the area immediately.”
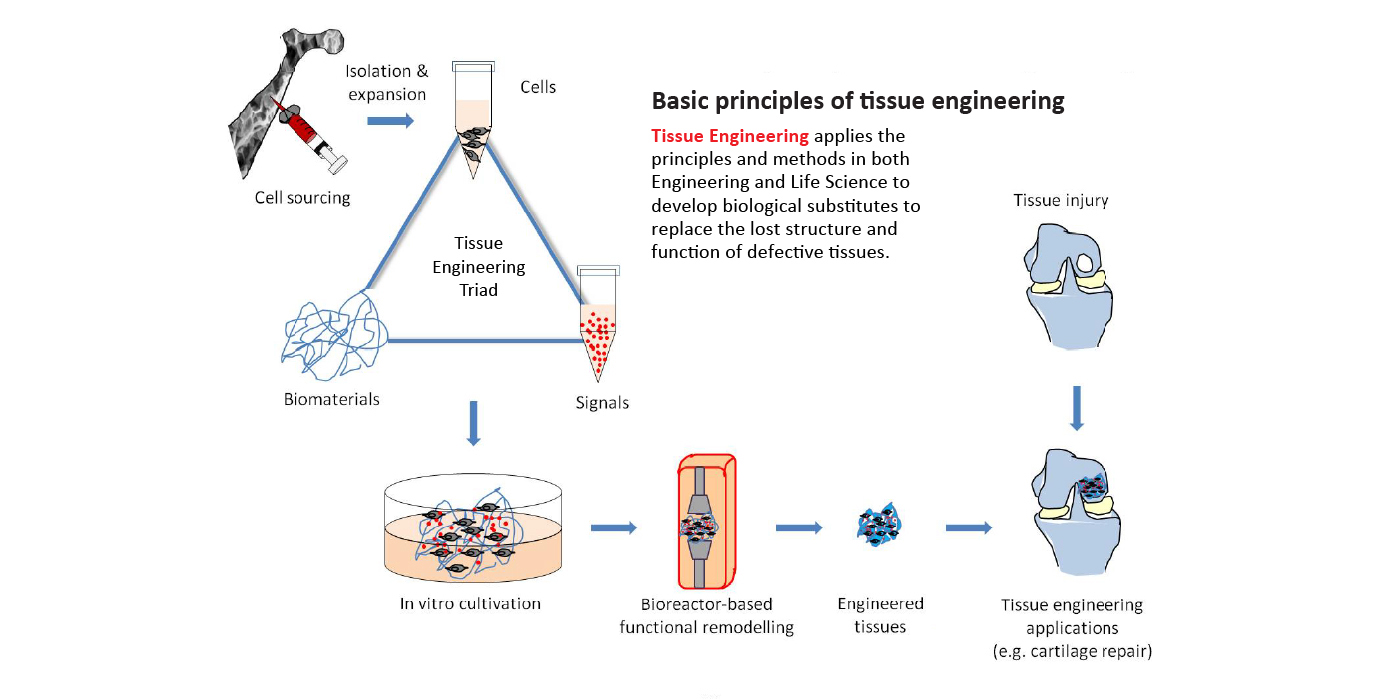

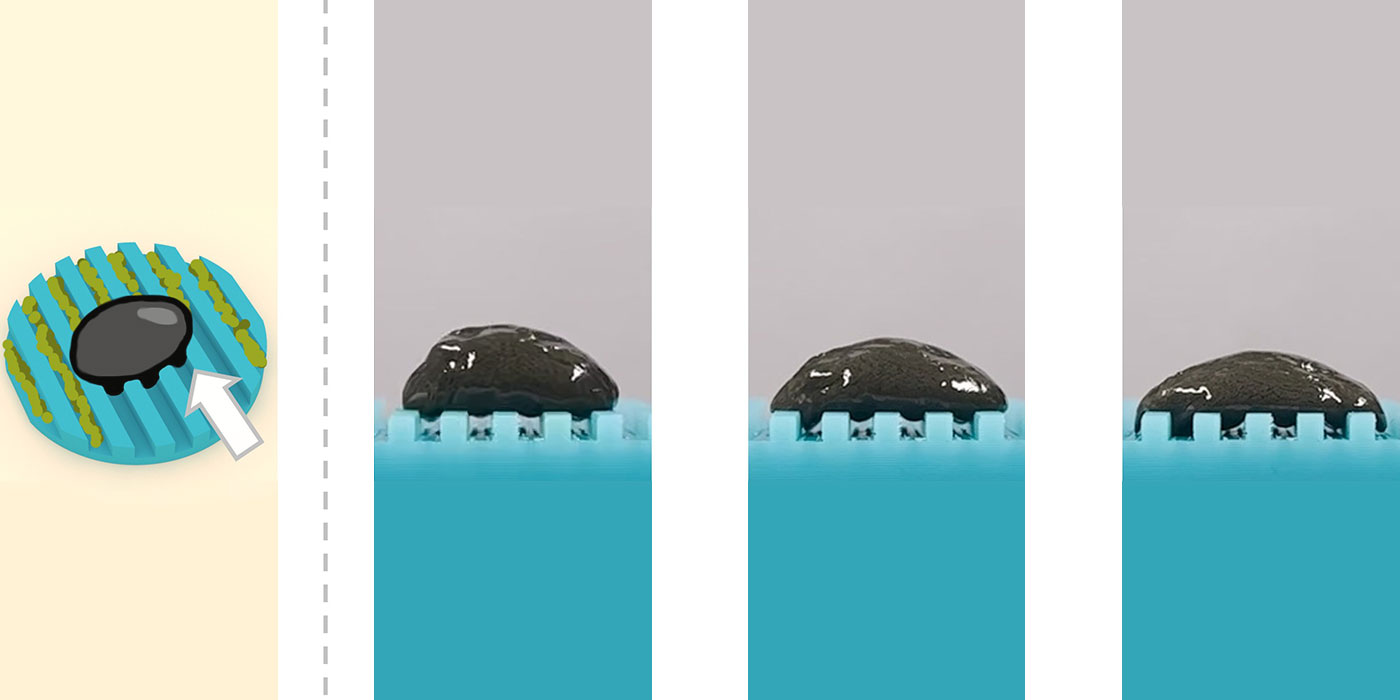
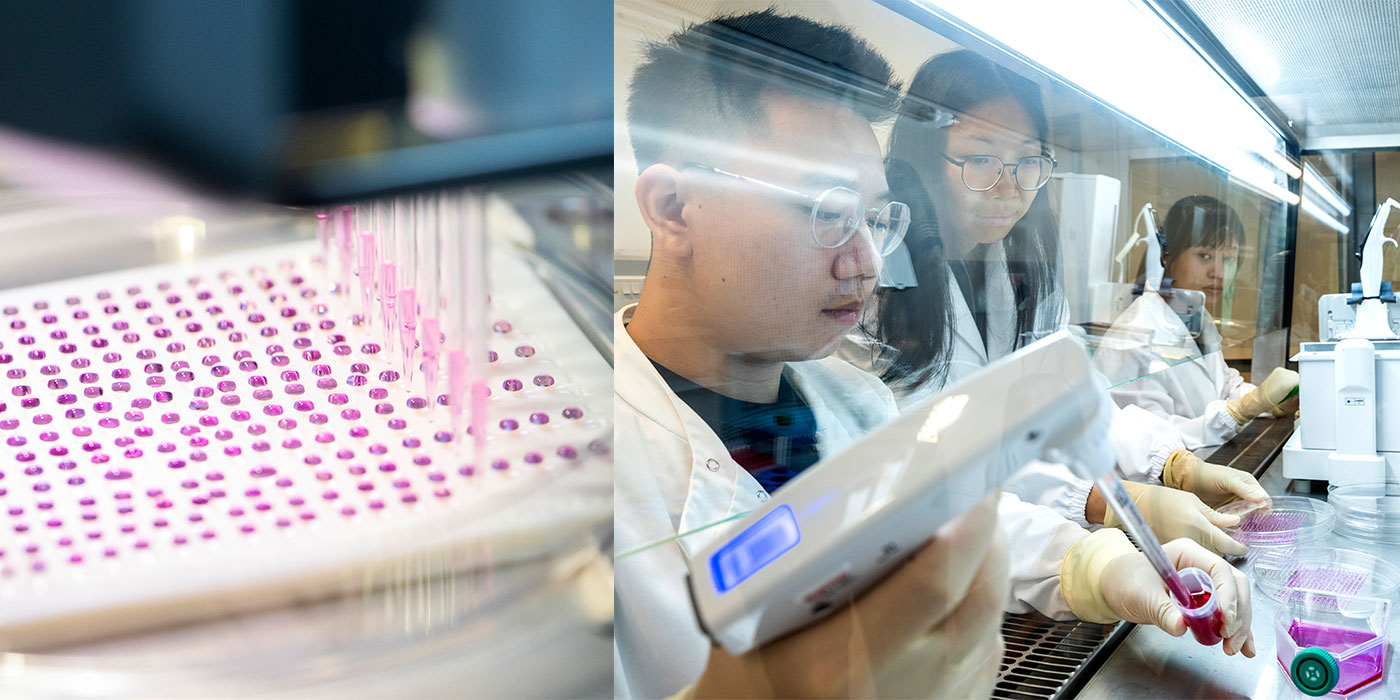
These regenerative complex tissue plugs allow orthopaedic surgeons to use the minimal invasive arthroscopy procedure to repair cartilage damage without the need to hurt the patient’s own cartilage, like the existing surgical procedures do. “We grow the cartilage tissues in vitro using the patients’ own stem cells and use the engineered cartilage to replace the damaged tissues. We are now translating this technology for use on humans,” adds Professor Chan. The performance of eOCT has been proven comparable with autograft transplantation in animal studies.
The breeding ground of innovation
Professor Chan is currently a professor in CUHK’s School of Biomedical Sciences, Institute of Tissue Engineering and Department of Biomedical Engineering. She obtained her bachelor’s degree in Biochemistry and her PhD in Surgical Science from CUHK. She was subsequently offered a postdoctoral fellowship in laser medicine at the Massachusetts General Hospital in the US. Before joining CUHK, she worked in the Biomedical Engineering programme of The University of Hong Kong. She is the first tissue engineering scientist to develop this technology to such an advanced stage.
The atmosphere of innovation, the multidisciplinary research culture and the research facilities at CUHK are the reasons for her homecoming. “The University values tissue engineering and regenerative medicine research, and multidisciplinary collaborations. The critical mass here, together with the visionary establishment of an ATP GMP manufacturing facility, is significant to tissue engineering research. I have collaborated with Patrick for many years. And I’m glad that we can translate eOCT technology into phase one of the clinical trial evaluating the safety of the technology.”
The eOCT treatment takes about four months to complete, which encompasses patient medical screening, bone marrow harvesting, sample transportation to Singapore’s GMP manufacturing facility, manufacturing eOCT in clean rooms, quality assurance tests by third party labs, minimal invasive arthroscopy and eOCT implantation by surgeons, followed by subsequent post-operation follow-up, data collection and analysis, for up to two years.
Locating a GMP facility that complied with Hong Kong regulations was challenging. She checked out cities like Beijing, Tianjin, Shanghai, Hangzhou, Xian and Guangzhou in her search for a feasible facility, but it turned out to be futile. “Due to regional differences in regulation of ATPs, the harvested samples processed in the mainland can’t be used for our clinical trials. We ended up opting a facility in Singapore, despite its longer turnaround time and higher cost,” Professor Chan elaborates.
With funding support from the RAISe+ scheme, she will set up the GMP manufacturing capability of eOCT in Hong Kong by working with the ATP GMP Centre of the Hong Kong Institute of Biotechnology (HKIB), so as to support subsequent clinical trials and commercialisation. The centre at the HKIB will provide a Pharmaceutical Inspection Co-operation Scheme GMP-compliant facility that produces clinical grade ATPs, including eOCT, for approved clinical trials and treatment.
The brave new world of personalised medicine
Professor Chan has established the Tissue Engineering Laboratory to improve patients’ quality of life by bioengineering biomaterials and stem cell-based tissues for personalised therapies. Her research interests include complex tissue engineering, natural biomaterials, organoids and tumoroids, mechano-regulation, cell-material interface, multiphoton microfabrication and micropatterning, as well as laser medicine.
Her dream is to realise personalised cartilage regeneration within the healthcare system. “Some day in the future, patients with cartilage injuries may send their pre-stored stem cells from cell banks to professional tissue growth service providers for their made-to-order personalised eOCT as their tissue engineering option for arthroscopy implantation. Hopefully, the eOCT ATPs will allow them to regain motility and enjoy their preferred lifestyles soon afterwards.”
To develop better therapeutics for patients suffering from joint problems, the team has overcome numerous technical and non-technical constraints, together with applying soft skills to cope with unexpected circumstances, in order to push scientific frontiers and bridge unmet medical needs. “Some challenges could be heart attack-triggering,” she says. “A manufacturing facility once indicated that they wouldn’t continue their work due to sudden local policy changes, which would result in them discarding patients’ samples.” Her team tried to preserve them at all costs. She says, smiling, “Our commitment to serving patients fuels our courage to grasp the nettle.”
By Jenny Lau
Photos by LCT
- Samuel Au powers the future of healthcare with cutting-edge technology
- Barbara Chan endeavours to use tissue engineering to heal patients
- Lam Hon-ming pioneers sustainable agriculture through soybean research
- Liu Yun-hui drives robots with 3D-vision
- Tsang Hon-ki on moving from lab to market
- Raymond Yeung innovates in network technology for a smarter future
- Engineer Zhao Ni’s journey towards wearable medical devices for all